Jeffrey Friedman ’77 is a distinguished biomedical scientist who has dedicated his career to unraveling the molecular mechanisms that regulate body weight. A professor and laboratory head at Rockefeller University, he has held a concurrent position as an investigator at the Howard Hughes Medical Institute since 1986.
In 1994, Friedman discovered leptin, a hormone secreted by fat cells that regulates food intake and energy expenditure and has powerful effects on reproduction, metabolism, other endocrine systems, and immune function. His groundbreaking research has helped demonstrate that obesity can be a result of metabolic and hormonal disruptions rather than a lack of willpower, and has opened obesity research to molecular exploration. In addition to providing a new target for treating obesity, the discovery of leptin has helped scientists develop treatments for other metabolic conditions, including certain forms of diabetes. Friedman is a member of the Rensselaer Alumni Hall of Fame.
Q: What inspired you to research the causes of obesity?
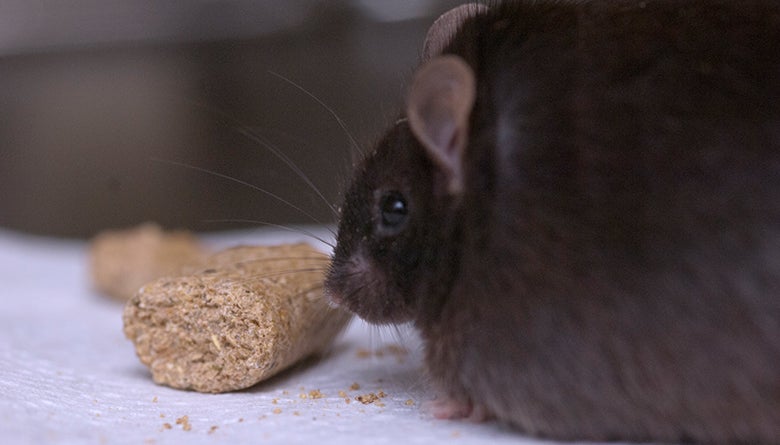
I was and continue to be interested in the neural mechanisms that control behavior. Early in my career, I learned about genetically obese ob/ob mice, which are massively obese because of a defect in a single gene. These animals are obese in part because they overeat voraciously. I thought that identifying the defective gene in ob/ob mice would provide an opportunity to study how feeding is controlled, as well as illuminating the pathogenesis of obesity.
Q: What was the first breakthrough you made?
It took eight years, but in 1994 we successfully identified the ob gene. I realized this in the middle of a May night when I developed an X-ray film that confirmed this and I remember the moment vividly. It was my Eureka moment. These data suggested that the ob gene encodes a hormone, leptin, that regulates food intake and body weight.
Q: How does a young researcher decide what to focus her or his research on?
Early in my career I came across an opportunity—in my case, it was the potential for solving the riddle of what causes obesity in ob mice—and pursued it. Very few ideas in science are unique. Rather, ideas float around until someone devotes themselves to pursuing it. In other words, in my view, success in science is recognizing a fertile line of research and pursuing it with passion and vigor, rather than thinking of an idea that no one else has considered (which seldom happens, if ever).
Q: What was the best advice anyone gave you?
Early in my independent career, without saying so explicitly, my mentor imparted the idea that I had to take full responsibility for the success of the project and not look to co-workers to overcome the various obstacles that inevitably present themselves.
Q: What is the next big breakthrough for obesity research?
Leptin acts on specific sets of neurons in the brain that regulate food intake, inhibiting neurons that increase food intake, and activating neurons that decrease food intake. This has led to the elucidation of a highly detailed wiring diagram of the neural circuit that regulates feeding. A key question now is how the many inputs that influence feeding in addition to leptin—smell, taste, emotional state, etc.—are integrated to generate a behavioral decision that leads an organism to either initiate feeding , or not.
There is typically a lag between a basic science advance and therapy and the hope is also that this work translates into new types of treatments. Leptin is already a treatment for lipodystrophy, a rare condition that can cause a severe form of diabetes. In addition, while most obese patients have high leptin levels, a subset of patients produce too little leptin. Recent evidence has suggested that patients with obesity and low leptin levels lose significant amounts of weight when given leptin.
Q: If you could ask people to change one thing in their everyday lives to benefit their health, what would it be?
The leptin system regulates weight and provides a biologic explanation for why some people are heavier than others. I find this explanation more satisfying than alternative explanations that posit that obesity reflects a loss of self-control . However, the system is not so precise that, with sufficient motivation (though even this is not always easy), one cannot lose modest amounts of weight, 7-10 pounds. This amount of weight loss is often sufficient to improve the health of obese patients with diabetes, hypertension, or other co-morbidities. So my advice is that people should not judge themselves too harshly if they are overweight or have difficulty losing weight; they are fighting against a powerful biologic system. However, if one is overweight with diabetes or other co-morbidities, he or she should do their best to lose a small amount of weight—which is achievable and capable of improving health—and not try to normalize their weight, which for most people is not realistic. In short, worry about your health, not your weight.
Read more:
https://www.newsweek.com/obesity-genetic-79383