By Torie Wells
For nearly six years, Pankaj Karande has been trying to solve a complex biological problem: How can science manufacture a skin graft that will effectively integrate with skin created by nature?
“As engineers working to recreate biology, we’ve always appreciated and been aware of the fact that biology is far more complex than the simple systems we make in the lab,” said Karande, an associate professor of chemical and biological engineering at Rensselaer Polytechnic Institute and a member of the Institute’s Center for Biotechnology and Interdisciplinary Studies. “We were pleasantly surprised to find that, once we start approaching that complexity, biology takes over and starts getting closer and closer to what exists in nature.”
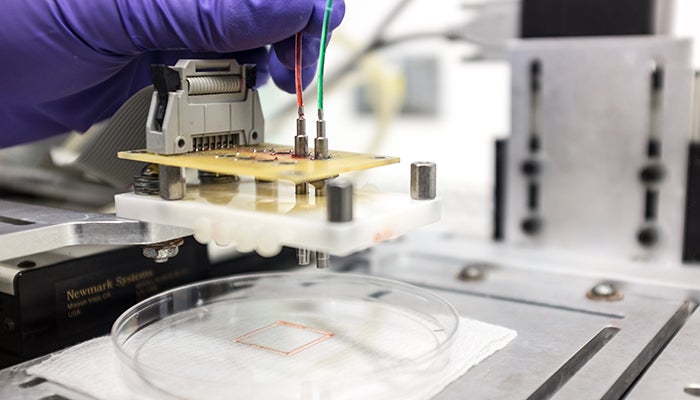
One barrier, which has historically prevented skin grafts from successfully integrating into the skin of patients, has been the absence of a functioning vascular system. To solve that problem, Karande and his team — working with researchers from Yale University — recently developed a way to 3D print living skin, complete with blood vessels.
This breakthrough is a significant step toward developing grafts that are more like the skin that the body produces naturally. While current clinical products may provide patients with some accelerated healing, they eventually fall off because they don’t have a way to integrate with host cells.
When the Yale team grafted the engineered tissue onto a special type of mouse, the vessels from the skin printed by the Rensselaer team began to communicate and connect with the mouse’s own vessels.
“That’s extremely important, because we know there is actually a transfer of blood and nutrients to the graft which is keeping the graft alive,” Karande said.
The next step for researchers will be finding a way to edit donor cells, using something like the CRISPR technology, so that the vessels can integrate and be accepted by the patient’s body.
He points out that more work will need to be done to address the challenges associated with burn patients, which include the loss of nerve and vascular endings. But the grafts his team has created bring researchers closer to helping people with diabetic or pressure ulcers.
“For those patients, these would be perfect, because ulcers usually appear at distinct locations on the body and can be addressed with smaller pieces of skin,” Karande said. “Wound healing typically takes longer in diabetic patients, and this could also help to accelerate that process.”
Watch Karande explain the development: